Sheffield family devastated after do not resuscitate decision made on ‘fit and healthy’ dad
and live on Freeview channel 276
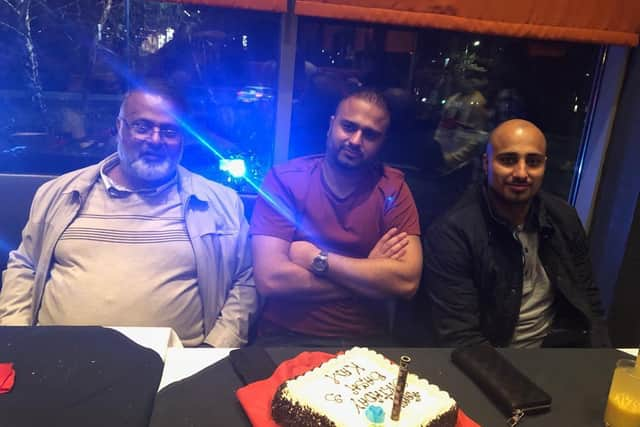
The family of Bashir Ahmed, 68, from Nether Edge said a Do Not Attempt Cardio-Pulmonary Resuscitation (DNACPR) decision was taken without his or their consent one day after the father-of-eight was admitted to the Royal Hallamshire Hospital on 2 October with coronavirus.
His son, Imran Ahmed, said: "We’re Muslim, we don’t accept DNACPR. Previously, I had faith in the NHS [...] and always held the NHS in high regard.
Advertisement
Hide AdAdvertisement
Hide Ad"My dad rang me distressed from his mobile phone [in hospital]. He said he had capacity to understand and be able to communicate with everyone.”

The Care Quality Commission (CQC) – England’s independent regulator of health and adult social care – said DNACPR decisions and advance care plans should only ever take place with clear involvement of the individual, or an appropriate representative, and a clear understanding of what they would like to happen.
Imran insisted his father, who was in remission from leukaemia, was ‘fit and healthy’ before catching Covid-19, but he died at the Hallamshire on 17 October following the decision not to resuscitate.
He added: "It wasn’t like he was away from it all, he was still waking up and going to work at 6am and coming back at eight or nine at night.
Advertisement
Hide AdAdvertisement
Hide Ad"I’m devastated, me, my family and everyone else. I can’t come to terms with it all. My dad was the heart and soul of our family and our business.”


Imran became so concerned about his father – a property developer who also ran a transport business – he phoned the police the night before he died.
South Yorkshire Police confirmed they were contacted on 16 October over concerns about the safety for a patient at the Hallamshire and officers “liaised with the hospital staff and ensured that the patient was safe.”
The family lodged a complaint with the hospital over Bashir’s treatment but have paused it while they seek further advice.
Advertisement
Hide AdAdvertisement
Hide AdIt comes after the CQC found evidence DNACPR orders were used without the input of patients or their families during the first wave of the pandemic. There is no evidence to suggest wrongdoing in Sheffield, however.


One carer told the CQC an on-call doctor informed care home staff an order would automatically be put in place if a resident caught Covid-19, while another witness said GPs told some care homes and learning disability services to place blanket orders on everyone in their care.
The CQC is now examining the practice at Sheffield Teaching Hospitals, which runs the Hallamshire, and six other NHS trusts across England as part of a wider investigation prompted by its findings.
A CQC spokesperson said Sheffield Teaching Hospitals has been chosen to cover a cross-section of areas and a mix of demographics. The final report is due to be published in February 2021.
Advertisement
Hide AdAdvertisement
Hide AdChrissy Meleady MBE, CEO of Equalities and Human Rights UK, said her organisation has directly intervened in cases where DNACPR orders have been made in Sheffield.


She added: “We welcome the CQC interim report and findings which vindicates our expressed concerns during the entire Covid period regarding the imposition of DNACPR orders”.
Sheffield Teaching Hospitals said they were unable to comment on this case but Dr David Hughes, medical director at the trust, said: “Our clinical teams work tirelessly to provide the best care possible for all our patients and thankfully the majority of patients never need to consider a DNACPR.
"Occasionally a patient will request not to be considered for Cardio-Pulmonary Resuscitation (CPR) and these decisions are explored with the patient to establish that they have the full information to make such a profound decision. Once this has been ascertained the patient’s decision is respected.
Advertisement
Hide AdAdvertisement
Hide Ad"Sadly there are times when despite the very best efforts of everyone involved, a patient’s clinical condition has deteriorated to such a point that it is necessary to consider whether or not resuscitation would be in their overall benefit should their heart stop. Any decision is based on the severity of the patient’s clinical condition, and whether attempts to resuscitate would be expected to succeed.
"Resuscitation is a traumatic event and the impact on a patient if it is unlikely to succeed also has to be taken into account. It may be that the patient would still be keen for CPR to be considered but the medical opinion is that it would be unsuccessful. In such scenarios this would be fully discussed with the patient and the family.
"A DNACPR decision is never taken lightly by anyone involved and takes into account all available information, not just one clinician’s opinion. Discussions and support are offered to the patient and their families where possible to ensure all questions and other issues can be addressed sensitively and honestly.
"The outcome of any discussions with the patient and all of the clinical information is then recorded in the patient’s notes to ensure everyone involved in the patient’s care is fully aware of the situation.”