Live updates from The Star's visit to a Sheffield GP surgery


Today The Star is visiting Birley Health Centre in Sheffield, to spend the day with Dr Ben Allen and the rest of the staff there.
We’ll be looking at how busy the GP surgery is, patient satisfaction with the services, and asking doctors and other medical staff what the job is like these days.
Advertisement
Hide AdAdvertisement
Hide AdThere has been a lot of frustration lately from doctors over the news stories published in national media and discussions in the House of Commons which falsely paint a picture of GPs lazily telling patients to sign up for online appointments or passing people on to other medical professionals.
And many patients have complained of difficulty getting appointments.
A number of Sheffield GPs have pointed out that, while patient’s anger is justified and they respect it, chronic underfunding of the NHS and the increased expectations of what it is GPs are supposed to cover in their remit has left doctors facing the impossible task of providing a health service that caters for what people want rather than what they need.
And the Government’s recent announcement of more funding for face-to-face appointments was slammed as ‘inadequate’ and plans to rank and fund surgeries based on how many face-to-face appointments they provide was branded ‘dangerous’.
Advertisement
Hide AdAdvertisement
Hide AdAnd many GPs have said this increased demand, along with the cutting of resources available to meet it, means they are working harder now than they have ever done in their lives.
Keep up-to-date with whet we learn using this live blog.
The Star spends the day in Sheffield GP surgery
Key Events
- GP surgeries and the services they provide has been a hot topic in the news in recent weeks
- The Government is encouraging doctors to provide more face-to-face appointments and has offered some funding
- However doctors say the funding is inadequate and that they do not have resources to meet demand
- Meanwhile, patients grow frustrated with the fact that doctors are not always able to meet them when they want
- Today The Star will be spending time at a GP surgery to see what it is like
What is it like being a GP at the moment?
In the past when The Star has spoken to GPs, some have suggested that the pressures of the job is causing some to reconsider their choice of career.
With the number of GPs in decline, this factor adds to the difficulties general practice already faces in the form of increased medical complexity and demand, and the lack of resources.
Dr Allen said: “It’s exhausting. When you see me you see a very different person at the end of each day compared to the start.
“But it is a privilege to support people who are ill, and patients on the whole are really pleased with the service they get here.
“Our workload has spiralled, medical complexity has spiralled and GP numbers are going down. That is why sometimes people can’t get appointments.
“I understand people being frustrated about that but it is not our fault.
“It is hard when the only time you get to reflect on the service the health centre provides, and how to improve it, is your time off, but that is what I have done and that is why I think we have done well.
“There needs to be changes, and I think general practice needs to better communicate these changes. We need to help patients to understand why we are working the way we are and show them the logic behind it.
“It is not as simple as somebody being ill and not being able to get an appointment. Most GPs are working really hard and they are exhausted and demoralised.
“Patients also need to be able to voice their anxieties so we can work together to improve the services GPs offer using systems that enable us to give people what they need.”
What is demand for GPs like and have patients been aggressive?
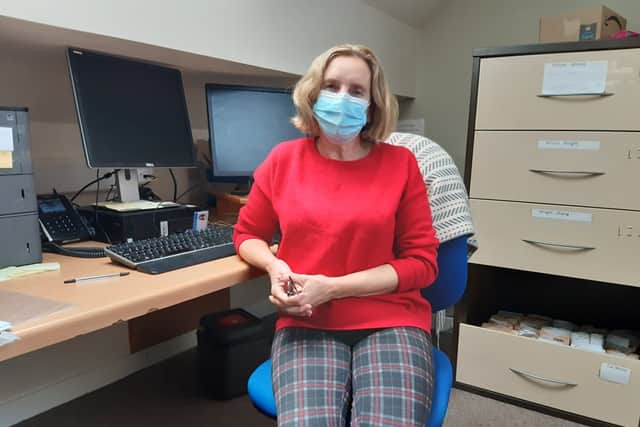

Sue Breeze, the patient liaison at Birley Health Centre, is the member of staff who deals with patient complaints, as well as helps decide which petients get to see which doctor, PA or nurse.
And having worked at Birley Health Centre for 17 years, she has seen first hand the changes in demand on GPs and how doctors can treat patients.
She said: “I worked on reception for 16 years and now I have moved into this role. I work alongside doctors and I enjoy being in the full of it.
“Demand has really increased and patients’ expectations have really increased. People who in the past might not have asked for face-to-face appointments are starting to ask.
“And I think this is because of what is being said in some of the media.
“We have people who would have sought help from a pharmacy first, or who might have self-managed asking for a GP now.
“Things have changed since Covid as well. People are scared they might have it and are rushing straight to a GP with things that they might have managed at home before.
“Covid has also meant that a lot more people are isolated and this has impacted mental health. People can’t visit their neighbours as they are scared stiff of catching Covid, and their family might live far away.
“This is a big concern at the moment, and more people have been getting in touch about things like social isolation since Covid.”
There have been occasions when patients of GPs in Sheffield have reportedly been angry and even verbally aggressive when they have been told they are unable to get a face-to-face appointment.
However, Dr Allen explained that with the increase in demand coupled with the increase in complexity of medical cases seen by GPs, it is not possible to see every patient in exactly the way they want, every time.
Ms Breeze also said that at Birley they have had no difficulties with patients becoming physically aggressive, and that it is important to be understanding if a patient is angry and verbally aggressive.
She added: “There are a few like that, but the vast majority are lovely and have sent us flowers and cards and all sorts.
“Problems with patients are nowhere near as bad as some of the media says they are.
“We have been open all the way through the pandemic. I think we have managed really well and I think patients have appreciated that.”
How is it decided who gets to see a GP?
Many patients who contact their health centre do so hoping that they will get to see a GP.
However, nowadays, a ‘triage’ system is in place which means that a patient’s condition is reviewed and then they are sent to the most appropriate medical professional.
This can be the GP, or a physician associate, a nurse or a specialist such as a physio.
Dr Allen explained how it is decided which patients see GPs, and which are sent elsewhere for treatment.
Birley Medical Centre is one of two in Sheffield - along with Pitsmoor - which uses a tool called ‘askmyGP’ to manage all its appointments.
Patients get in touch either through the Birley Health Centre website, or by phoning up, and explaining their complaint. This is then entered into the askmyGP system where a member of staff who is doing the triaging - often the on-call doctor and a member of administrative staff - will assess it.
They then decide - based on things like who the patient has seen before and members of staff’s workloads - who can best deal with the issue at hand.
Dr Allen said: “Continuity is important. We always want people to see the same people when we can. If the last person they saw is not in, then we see if they can wait, and if they cannot we arrange for them to see somebody else.
“A patient will get in touch and often a person in admin will decide who is the best person a patient will see.”
When asked about the fact some patients being angry about an admin staff member deciding they should not see a GP straight away, Dr Allen said: “For a start, the admin knows a lot better than the patient.
“They know who is in that day and they know what people are able to do.
“Patients can be sent to a PA or a nurse, but that does not mean that they will not at any point be seen by a GP.
“And, for example, if a PA feels like they need a GP to see a patient, they can refer them to one. Or they can have a patient come in and a GP can also go into the appointment as well.
“But we need to make sure people are sent to the most appropriate person.
“If 20 people rang up and asked to see Dr Allen and they all got that no matter their condition, and then another person who needed a GP urgently rang up later and I was busy, the person who was more urgent would have to be told to try again the next day.
“That is not a good way to try to make sure people get what they need.”
How many patients get face-to-face appointments?

In recent weeks, GPs have come under a lot of criticism from the Government and some members of the public over the perceived ‘difficulty’ in getting a face-to-face appointment.
However, many doctors have explained that it is a minority of patients who feels this way.
And today, Dr Ben Allen has shown that the reality is that more patients get seen face-to-face than the number who ask for that.
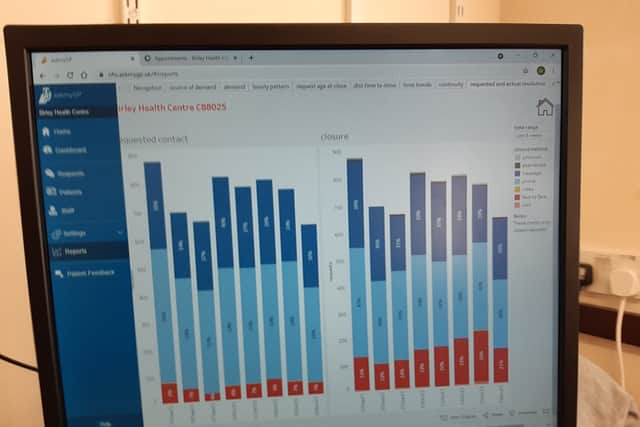
The Star has seen the data for the patient appointment requests that have come into Birley Health Centre over the past eight weeks.
Since September 13, around eight per cent of patients who requested an appointment at Birley asked for a face-to-face meeting with a medical professional.
Meanwhile, 56 per cent requested an appointment over the phone, and 36 per cent asked for help to be sent via email.
What actually happened over those eight weeks was that on each day since September 13 between 15 and 26 per cent of patients who requested appointments have been seen face-to-face.
And on any given day between 30 and 40 per cent of patients were dealt with over the phone or by email.
Dr Allen explained: “Email is usually the most efficient way to help somebody, but there will be some patients who need face-to-face. And in some cases, a patient will ask for a phone call or an email and we will tell them that they need to come in.
“More important than efficiency, though, is helping people using the right method. It is not efficient to get it wrong.
“Equally, it is important not to give sombody a face-to-face appointment who does not need it, so we say we will call them instead. In those cases, we may not be giving one person exactly what they want, but in doing that we ansure we have the time to give a number of other people what they need.”
Examples given today include a two-month-old baby with a cough and wheezing, whose family asked for an email appointment. Dr Allen has instead asked them to attend a face-to-face appointment. Another was somebody who wanted to be seen face-to-face for Athlete’s Foot, who was instead told to go and see a pharmacist.
Dr Allen added: “We will always do what is needed. If we just let the first patients who rang up have a face-to-face appointment then we would only see half the people that we manage to see this way.
“We also try to see everybody on the day they ask to be seen. If somebody gets in touch with us between 8am and 1pm they will almost certainly be seen to that day. And if they get in touch after that and it is urgent we will try and see to them, too.”
How busy are GPs?


The first job at a GP surgery is to allocate the patient requests for appointments to the various members of staff at work that day.
This can include GPs, physician associates (PAs), nurses and administrative staff, and who sees each patient depends on the treatment a patient requires.
Today (Friday, November 5) at Birley Health Centre Dr Ben Allen has said that they expect to see around 124 patients. The capacity of the health centre, based on the number of staff they have available, is 100.
Today the health centre is fully staffed, with five doctors and two PAs working. This means 100 is the maximum capacity at Birley on any given day - which Dr Allen describes as the amount GPs can ‘comfortably see’.
However, the number of patients seen is consistently far higher than that - a sign of the NHS being overstretched that Dr Allen says is ‘typical’ of most GP surgeries in Sheffield.
On most days, the surgery is seeing around 50 more patients than it has capacity for, with Monday usually being the busiest day where around 27 per cent of the week’s patients are seen, which equates to 220 appointments.
On other days, Dr Allen says the average is about 150.
By 8.30am this morning, 17 patients had already been seen at the surgery.
Dr Allen said: “Today is okay. We have got nobody off ill and nobody on holiday, and I can’t remember the last time we had that.
“I have had Fridays where we have been short staffed, as I have had to pull a person off a Friday shift to fill a gap on another day.”
On top of the expected 124 appointments expected to be carried out by Birley Health Centre staff today, the staff must also deal with 60 blood tests and 68 prescriptions.
They must also deal with letters that come in from other health services such as A&E, hospitals and mental health services, which ask them to see more patients, and any number of ‘tasks’ that come in, which can include jobs related to the day-to-day running of the surgery. There are also home visits to carry out.
Dr Allen estimated that on average he works 11 hour days, and does around 40 ‘jobs’ a day when all of the above are taken into account.
And Dr Allen added that a ‘misunderstanding of general practice’ adds to the pressure on GPs, with even more work being sent their way and expected of them.
This ‘misunderstanding’ is even present within the NHS itself. At the moment, the NHS app tells people that they can contact their GP to get results from tests done in hospitals, Dr Allen says.
“That is incorrect,” he said. “How we can do that is beyond me. A test is carried out by somebody to answer a question they are asking.
“The results of a test can only be explained to a patient by a person who decided to do the test and knwos exactly what questions are trying to be answered.”
Sheffield GP slams Government £250m ‘boost’ for extra patient appointments as not enough


A Sheffield doctor has dismissed the Government’s announcement to provide more funding to help ‘improve access’ to appointments as ‘unhelpful’ and says it is likely to make the service provided by GPs worse rather than better.
In October, Health Secretary Sajid Javid announced a £250 million ‘winter access fund’, aimed at enabling GP practices to improve availability and increase the number of face-to-face appointments and same-day care.
The new investment will fund locums as well as support for GPs from other health professionals such as physiotherapists and podiatrists.
However, the investment comes in tandem with a scheme where GP surgeries that fail to provide an appropriate level of “access” will be named and shamed in league tables as patients are given a new right to demand face-to-face appointments.
And practices which fail to provide an ‘appropriate’ level of face-to-face appointments will not be eligible for the new funding.
The proposals have been condemned by swathes of medical professionals for being making unrealistic demands of an overstretched service, as well as opening GPs up for more abuse as they try to cope with the backlog brought on during the pandemic, as well as increasing demand on their services.
Sheffield GP calls for more Government funding for NHS before it’s too late


A Sheffield doctor has spoken out to address the complaints GPs often field, including issues with waiting times and difficulties around appointments.
Dr Alison Hobbs, who works at Pitsmoor Surgery, echoed points made by Birley GP Ben Allen earlier this year and focused on funding and resource shortages, increasing workloads and a backlog of patients that has built up over the pandemic in her explanations for the way GP services currently are.
Dr Hobbs said: “I think a lot of the criticism is justified. We are angry on behalf of our patients. People don’t see how frustrating it is for us to know that we are not providing the services we want to and we are having to make further cuts.
Sheffield GP warns ‘there’s a pandemic out there still burning’ after being confronted by ‘angry’ patient

A Sheffield GP has warned that the Covid pandemic is far from over after being confronted by an ‘angry’ patient over delays.
Dr Andrew Lee is concerned that the Government is sending out the wrong message ahead of so-called ‘Freedom Day’ tomorrow, Monday, July 19, when Covid restrictions are set to be removed despite infection rates and hospital admissions rising across the UK.
Dr Lee, who is also a reader in public health at the University of Sheffield, said: “Had an angry patient in clinic yesterday when I told him delays likely for hospital referrals. He thought July 19 meant everything is back to normal.
Why it’s so hard to get a doctor’s appointment in Sheffield: GP lifts lid on ‘frantic’ NHS pressure


Amid increasing complaints from patients about difficulties securing appointments with GPs in Sheffield during and after lockdown, one doctor in the city has opened up about the pressures practices face.
Dr Ben Allen, GP Partner Birley Health Centre, wrote a public ‘apology and explanation’ and posted it on social media, in which he outlined the reasons why GPs were struggling with workloads, and also sought to dispel some of the ‘myths’ circulating about the care GPs are able to give.
Now, Dr Allen has spoken to The Star to give a more in-depth doctor’s perspective on the issue.
